PATIENT RESOURCES:
Skin Cancer: Prevention, Risks, and Early Detection
Navigating the risks and prevention of skin cancer can feel overwhelming. Do you really need to be concerned? Are you or your loved ones at risk? What should you be looking for on your skin to stay safe?
You’re not alone in these concerns. According to the American Cancer Society, the incidence of skin cancer is on the rise in the U.S., with more cases diagnosed annually than all other cancers combined. But the good news is, when detected early, skin cancer is highly treatable.
There are plenty of ways to stay proactive with prevention and early detection. By learning what to look for and taking steps to protect yourself and your family, you can take charge of your health. Whether you’re scheduling a full-body skin exam or seeking advice about a suspicious spot, we’re here to help.
Our goal is to provide you with peace of mind through education, prevention, and early detection.
Skin Cancer FAQs
Am I at Risk for Developing Skin Cancer?
Exposure to ultraviolet (UV) radiation from sunlight, tanning beds, and lamps significantly raises your risk of developing skin cancer. Click here for more information about UV radiation.
Although anyone—regardless of ethnicity or skin color—can develop skin cancer, some characteristics and medical factors can increase your risk:
- Fair skin, light-colored eyes, and blonde or red hair
- A history of sunburns or skin that burns easily
- A personal or family history of skin cancer
- Having many moles or freckles
- Previous radiation therapy
- A weakened immune system (due to conditions like HIV, organ transplants, or certain medications)
- Certain medications that increase sun sensitivity
If you have any concerns about your medications or other risk factors, talk to your doctor for personalized advice.
How Do I Prevent Skin Cancer?
The best way to prevent skin cancer for yourself and your family is through proper sun protection. While starting from birth is ideal, it’s never too late to begin taking steps to safeguard your skin.
Here are some key tips:
- Avoid the sun during peak hours (10 a.m. to 4 p.m.) when UV rays are strongest.
- Choose tightly woven clothing that blocks sunlight. Hold the fabric to light—if you can’t see through it, it offers better protection.
- Apply sunscreen with at least SPF 30 whenever you’re outside, even on cloudy days. Reapply every two hours or after swimming or sweating.
- Wear sunglasses that offer 100% UVA and UVB protection to shield your eyes and the delicate skin around them.
By taking these precautions, you’ll reduce your risk of skin cancer and keep your skin healthier in the long run.
How Do I Identify a Suspicious Lesion?
Knowing your skin and recognizing what’s normal for you is essential. Monthly self-skin examinations can help you spot any unusual changes early. All you need is a mirror and a good look at your skin.
Regularly checking your body for new growths or changes in existing moles is key to identifying suspicious lesions. If you notice anything new, changing, or growing rapidly, consult your doctor or dermatologist right away.
By combining monthly self-examinations with routine check-ups from your dermatologist, you can greatly increase the chances of detecting skin cancer early and treating it effectively.
During your self-examination, be on the lookout for:
- Changes in the size, shape, or color of a mole or growth
- Lesions that are rough, oozing, bleeding, or scaly
- A sore that won’t heal
- Pain, itching, or tenderness in a lesion
Taking time to know your skin could be a lifesaving habit.
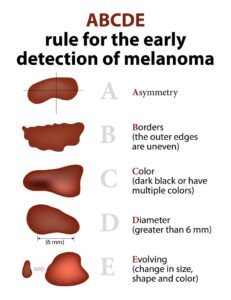 Use the following guidelines to help identify areas on your skin that you should discuss with your doctor:
Use the following guidelines to help identify areas on your skin that you should discuss with your doctor:
- Asymmetry: One half of the lesion doesn’t match the other.
- Borders: The edges are blurred, uneven, or irregular.
- Color: The color isn’t uniform and may include shades of black, brown, red, or white.
- Diameter: The lesion is larger than 6 millimeters (about ¼ inch) across.
- Evolving: The mole changes in size, shape, or color over time.
By keeping these guidelines in mind, you’ll be better equipped to catch suspicious lesions early and seek timely medical advice.
What are the Types of Skin Cancer?
Basal Cell Carcinoma
Basal Cell Carcinoma (BCC) is the most common form of skin cancer, known for being slow-growing and the least invasive. While BCC can extend into local nerves and cause damage, it rarely spreads to other parts of the body. Even though it grows slowly and is less likely to metastasize, early treatment is crucial to prevent further local damage. The good news is that when caught early, the cure rate for BCC is very high. Treatment options vary based on the size and location of the cancer and can be discussed with your dermatologist.
Squamous Cell Carcinoma
Squamous Cell Carcinoma (SCC) is the second most common type of skin cancer. If left untreated, actinic keratosis—often a precursor—can develop into SCC. This type of cancer typically appears as a red bump or scaly patch, particularly in areas with chronic sun exposure. Without treatment, SCC can grow larger and potentially spread to the lymph nodes. Fortunately, when caught early, SCC has a high cure rate. Treatment options vary based on the cancer’s size and location, and these can be discussed with your dermatologist.
Malignant Melanoma
Malignant melanoma is the most aggressive form of skin cancer. If left untreated, it can metastasize to other parts of the body. However, when caught early, melanoma is very treatable and often has a good prognosis. Unlike other skin cancers, melanoma can develop from a preexisting mole or appear as a new growth. Regular self-examinations are essential, as changes in a mole’s size, shape, or color could signal melanoma. If you notice any changes in your moles, see your dermatologist promptly. While not all changing growths are melanoma, it’s important to have them checked by a professional.
Actinic Keratosis (AK)
Actinic keratosis (AK) is a pre-cancerous skin condition characterized by small, pink, gritty spots, often found on sun-exposed areas like the head, neck, and hands. These spots feel like fine sandpaper. Since AKs can develop into squamous cell carcinoma (SCC), they are typically treated.
Treatment decisions depend on the number, location, and thickness of the AKs, as well as factors like season and personal circumstances. Your dermatologist will help determine the best option for you.
Mohs Surgery Helpful Information:
Mohs Surgery: What to Expect
There are several treatment options available for skin cancer, but Mohs surgery is considered the gold standard for many cases, particularly those located on the head and neck. It is also used in specific situations elsewhere on the body, such as when the cancer is large or has recurred after previous treatment. If your biopsy results indicate skin cancer and Mohs surgery is recommended, our team will be happy to discuss your options with you and determine if Mohs is the best choice for your situation.
It’s important to understand that, although Mohs surgery is performed in an office setting, it is still a surgical procedure, and patients should plan accordingly. Most Mohs surgeries are completed by mid to late afternoon, and many patients prefer to take the rest of the day off from work.
Mohs surgery is safely and comfortably performed without the need for a hospital or ambulatory surgery center, making the experience more efficient, comfortable, and cost-effective. The procedure is done under local anesthesia, and our skilled team ensures the anesthesia is administered as comfortably as possible. We also use a long-acting anesthetic to keep the area numb throughout the day. If you feel you may need additional relaxation, a mild sedative prescription can be provided at your consultation.
On the day of surgery, most of your time will be spent waiting for lab results and preparing for any necessary repairs. We recommend bringing snacks and entertainment to pass the time while you wait in our comfortable, welcoming waiting rooms. Many patients also use headphones during the procedure. On average, patients spend about 4 to 6 hours in the office, though we ask that you reserve the entire day to ensure thorough treatment of your skin cancer.
After surgery, a pressure dressing is typically applied to the surgical site, which can often be removed after 24 hours. Surgical tape is usually placed over the incision line(s) to protect the area. Our team will provide detailed instructions on how to care for your surgery site and give you written instructions to take home. Please arrange for someone to drive you home after surgery. Your companion is welcome to wait in our office or provide a mobile number to be contacted when your procedure is complete.
Pre-Surgery Instructions:
These instructions are intended for patients of Advanced Dermatology & Skin Surgery and are not meant to be comprehensive. If you have any questions or concerns, please contact our office at 828-210-7989.
If you have a surgical procedure scheduled with one of our providers, please follow these guidelines to minimize the risk of complications before, during, and after your surgery.
Bleeding Complications:
Certain medications can increase the risk of bleeding during surgical procedures. Please follow these guidelines:
- Anticoagulants (blood thinners):
If you are taking aspirin, Plavix (clopidogrel), Coumadin (warfarin), Pradaxa (dabigatran), Xarelto (rivaroxaban), or Eliquis (apixaban), it’s important to consult with your doctor before stopping any medications. If taking aspirin as a preventative measure, discontinue it 10-14 days prior to surgery unless instructed otherwise. You may resume aspirin 72 hours after surgery. - Ibuprofen and NSAIDs:
Medications like ibuprofen, Advil, Aleve, Celebrex, and other non-steroidal anti-inflammatory drugs (NSAIDs) should be discontinued 3 days before surgery, if possible. Acetaminophen (Tylenol) may be taken if needed. - Supplements and Alcohol:
Vitamin E, multivitamins, fish oil, and alcohol may increase bleeding. Please discontinue them 3 days prior to your procedure, and you may resume them the day after surgery.
If you are taking any of these medications as prescribed by your physician, continue them unless advised otherwise by our office.
Infection Prevention:
Skin infection is a potential risk with any surgery, but you can minimize the chances of infection by following these steps:
- If you have a history of infections after surgery, let us know; oral antibiotics may be prescribed before the procedure.
- On the day of surgery, cleanse the surgical area with soap and water (use antibacterial soap if available).
- Avoid wearing cosmetics if the surgical area is on the face.
- Do not shave the area the morning before surgery, as this can increase the risk of infection. If needed, we will shave the surgical site just before the procedure.
Surgical Pain:
Mohs surgery is performed safely under local anesthesia, meaning you will be fully awake but will not feel pain during the procedure. If more than one sample is needed, we will reapply anesthesia to ensure the area remains numb throughout the day. We also use a special long-acting anesthetic to prevent numbness from wearing off during any wait times. If a repair is necessary after the tissue removal, a local anesthetic will be used for that as well. Our goal is to make sure you are comfortable and pain-free during both the surgery and any required repair work.
After surgery, most patients experience only minor discomfort, which typically subsides quickly. However, pain levels can vary depending on the extent of the procedure. To help with any discomfort, a prescription for pain medication will be provided after surgery, if needed.
Recovery After Mohs Surgery
To aid in your recovery, keep the dressing dry for 24 hours, so it’s a good idea to shower before your appointment. We also suggest avoiding heavy lifting or strenuous exercise for about a week after surgery, though light activity like walking is fine. If your job involves physical exertion, consider adjusting your work schedule accordingly. If that’s not feasible, please discuss options with our surgery team. For non-physical jobs, you may feel well enough to return to work as soon as the day after the procedure. However, visible swelling, bruising, or surgical dressings might influence your decision, so feel free to consult with our staff about what to expect.
Swelling and bruising near the surgery site are common but usually resolve within several days. Using ice packs can help reduce swelling and speed up recovery.
Post-Operative Activity Restrictions:
To ensure proper healing, follow these guidelines after your surgery:
- Limit physical activity for 24-48 hours post-surgery.
- Avoid lifting anything heavier than 10 pounds for at least one week.
- Any activity that raises your blood pressure could cause post-operative bleeding. After 48 hours, your activity restrictions may vary depending on the surgical site and whether you have stitches. Consult with your provider for specific recommendations.
If you have a scheduled activity that may interfere with your healing, consider postponing your surgery to avoid complications.
For any questions, feel free to call our office at 828-274-4880.
What if I have scarring from MOHS surgery?
If you have scarring from Mohs surgery, it may be beneficial for you to have a consultation with our Aesthetics team. Learn more about our aesthetic dermatology services here.

Medical records release form
Click here or the form image to download our medical records release form. You can print and fill out before your next appointment.